Fertility Treatments
Once you have undergone your fertility investigations, you may begin considering the fertility treatment options available to you. Depending on the cause of your fertility problem, your fertility team may recommend a type of treatment called assisted reproductive technology (ART). Here, you will find more information on the options that may be available to you, and what to expect with each treatment.
Fertility treatment explained
Fertility treatment options
There are three main treatment options that may be offered to individuals or couples seeking fertility treatment:1
1. Fertility drugs
Medication to help induce ovulation can be offered to women trying to conceive naturally, as well as those undergoing ART.
Women with polycystic ovary syndrome (PCOS) may be offered clomifene citrate, metformin, or a combination of both.2 Gonadotrophins (are a group of hormones) may also be given to women who have an ovulation disorder that affects the release of hormones from their brain.3
2. Surgery
Men who have no sperm count due to an obstruction in their epididymis (the tube that carries sperm from the testes) may be offered surgical correction to help improve fertility. Women who suffer from conditions such as endometriosis, mild tubal disease, or a build-up of uterine scar tissue, may also be offered surgery to help improve their chances of pregnancy.1
3. Assisted Reproductive Technology (ART)

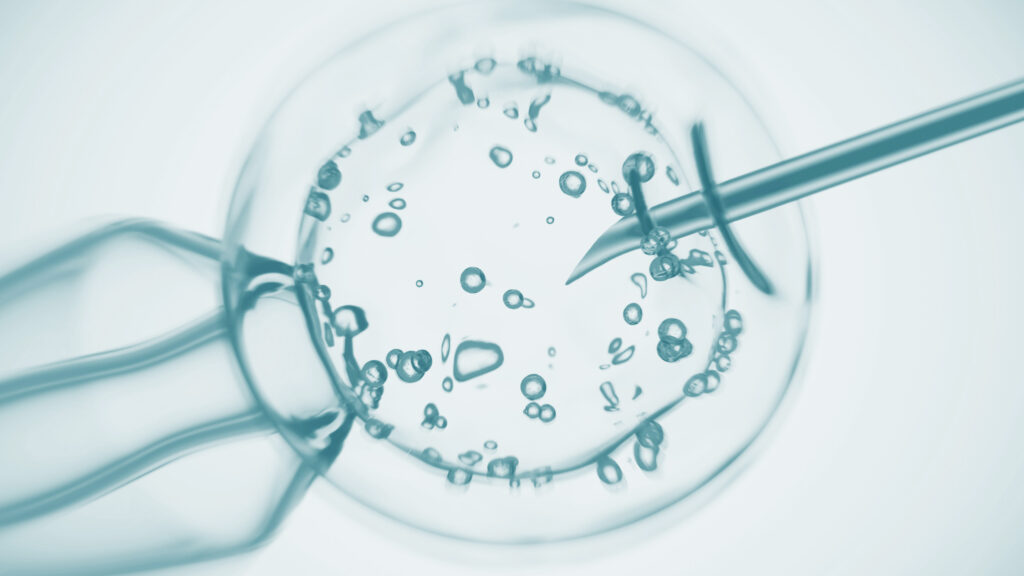
What is IVF?
IVF is a common fertility treatment option that involves the fertilisation of eggs with sperm, outside of the body.1 It is used for a variety of patients, from women affected by endometriosis to those with ovulatory dysfunction, and has demonstrated excellent success rates.4
What does a full cycle of IVF involve?
The stages of an IVF cycle will vary depending on the protocol used. However, they will typically include:
What does a full cycle of IVF involve?
The stages of an IVF cycle will vary depending on the protocol used. However, they will typically include:



1. Pre-treatment
Purpose: to improve response to hormone therapy, minimise the risk of an ovarian cyst forming, and help ensure that the timing of egg collection coincides with the availability of clinical and laboratory staff.1
Involves the administration of medication in the
form of a combined oral contraceptive pill, progestogen, or oestrogen, before ovarian downregulation or stimulation.1
2. Downregulation
3. Controlled ovarian stimulation
4. Ovulation trigger
5. Egg and sperm retrieval
6. Embryo replacement
7. Luteal phase support
Other fertility treatment options
Intrauterine insemination (IUI)
Intracytoplasmic sperm injection (ICSI)
Sperm and egg donation
| Treatment type | Whom may it be offered to? | Differences to IVF |
|---|---|---|
| Intrauterine insemination (IUI) |
People with:1
|
|
| Intracytoplasmic injection (ICSI) |
People with:2
|
|
| Sperm donation |
|
|
| Egg donation |
|
|
| Treatment type | Whom may it be offered to? | Differences to IVF |
|---|---|---|
| Intrauterine insemination (IUI) |
People with1:
|
|
| Intracytoplasmic injection (ICSI) |
People with2:
|
|
| Sperm donation |
|
|
| Egg donation |
|
|
Can IVF work for me?
The chances of success with IVF depend on multiple factors. These include the age and hormone levels of the female partner, the quality and quantity of eggs remaining in the ovaries, how long the individual or couple have been experiencing fertility problems for, and sperm quality of the male partner. 11, 12
IVF is a suitable treatment option and is the most effective form of fertility treatment for couples with infertility.4 However, every couple and individual are different and therefore will have varying rates of success. The National Institute for Health and Care Excellence (NICE) recommends three cycles of IVF as it is both cost-effective and clinically effective for women under the age of 40, with the cumulative effect of three cycles of IVF increasing the chances of a successful pregnancy to 45-53%.13
Anti-Müllerian Hormone (AMH) testing
Do you need to be a certain age to be eligible for IVF?
The effect of maternal age on the average rate of pregnancy
Annual Fertility Rate (per 1000 married women not using contraception)*
No Data Found
No Data Found
*Calculated on the basis of studies in 10 different populations that did not use contraceptives.17
Adapted from: Heffner LJ., N Engl J Med 2004.17
What can I do to improve my chances of success?
- Following a healthy diet.19
- Maintaining a healthy body mass index (BMI).19
- Engaging in moderate physical activity.19
- Looking after your mental wellbeing e.g., practicing mindfulness.19
- Reducing alcohol intake (this is applicable to both male and female partners).20
- Increasing intake of vitamin D21and E.22
What are the risks of IVF?
Although IVF is a very safe treatment option, it is still important to be mindful of the potential associated risks.
1. Medication side effects
2. Multiple births
3. Ovarian hyperstimulation syndrome (OHSS)
4. Ectopic pregnancy
Financing IVF
Is IVF available on the NHS?
How many IVF cycles can I have?25
According to NICE, the NHS should offer women under 40 three cycles of IVF treatment if they meet the following criteria:
- They have been trying to conceive through regular unprotected intercourse for two years.
- They have had 12 cycles of unsuccessful insemination, with at least six of the cycles using IUI.
- If the woman turns 40 during a cycle, they should complete their treatment but not be offered further cycles.
- They have had 12 cycles of unsuccessful insemination, with at least six of the cycles using IUI.
- They have never had IVF treatment before.
- They show no evidence of low ovarian reserve.
- They have been informed of the additional implications of IVF and pregnancy at this age.
Additional criteria may need to be met depending on decisions made by the CCG in your local area. If you are ineligible for NHS-funded treatment, you can pay to have IVF at a private clinic.8 There is normally no limitation on the number of cycles a patient can have at a private clinic.
Funding IVF privately
Better conversations with your doctor
Before your appointment
Before your appointment
When you are preparing to attend your first fertility consultation, the whole process may feel overwhelming. However, speaking directly with your doctor can be a great opportunity to discover more about the IVF process and to help you feel more confident about what to expect in your fertility journey.
To get the most out of your appointment, it can be a good idea to make a note – either on your phone or in a notebook – of any important questions you would like to ask your doctor and bring this with you to your consultation.
Additionally, your clinic may request that you have some preliminary tests, such as a blood test or a semen analysis, that your doctor can use to discuss a more personalised treatment pathway with you.
During your appointment
During your appointment
When you attend your initial consultation with your doctor, it is useful to bring along any prepared questions you have with you to help guide your conversation.
Initially, the doctor will talk you through the full IVF process, including required tests and medications, which may answer some of the concerns you have. Afterwards, if you still have any unanswered questions, you should feel free to ask your doctor about these to help familiarise yourself with the treatment journey and help you to know what to expect.
After your appointment
After your appointment
After you have attended your initial appointment, you should hopefully have a clear view of what to expect if you decide to go forward with treatment. You should have been given clear guidance on the next steps to take, including what tests you may need to book. If you have any further questions following your appointment, you should get in touch with your clinic who should be happy to answer these for you.
Useful questions to ask
Some commonly asked questions include:
- What tests are required before I can start IVF treatment?
- What are my chances of success with IVF?
- What can I do to increase my chances of achieving a successful pregnancy?
- How long does a treatment cycle last?
- How many treatment cycles will I need?
- What are the possible risks or side effects associated with IVF?
- How much does IVF treatment cost?
- What are my options if treatment fails?
- How soon can I try again?
Interview with Sophie, an IVF patient who talk about the stages of the IVF process and her own journey
Where is my nearest clinic?
- National Collaborating Centre for Women’s and Children’s Health (UK). Fertility: Assessment and Treatment for People with Fertility Problems. London: Royal College of Obstetricians & Gynaecologists; 2013. Available from: https://www.ncbi.nlm.nih.gov/books/NBK247932/ [Last accessed: December 2023].
- National Institute for Health and Care Excellence. Fertility problems: assessment and treatment. Available at: https://www.nice.org.uk/guidance/cg156/chapter/recommendations [Last accessed: r 2023].
- Messinis IE. Ovulation induction: a mini review. Human Reproduction 2005;20:2688-2697. Available at: https://academic.oup.com/humrep/article/20/10/2688/603349?login=true [Last accessed: December 2023].
- Huang JYJ, Rosenwaks Z. In vitro fertilisation treatment and factors affecting success. Best Practice & Research Clinical Obstetrics and Gynaecology 2012;26:777-788. Available at: https://www.sciencedirect.com/science/article/pii/S1521693412001393 [Last accessed: December 2023].
- El-Shawarby SA, Margara RA, Trew GH, Lavery SA. A review of complications following transvaginal oocyte retrieval for in-vitro fertilization. Human Fertility 2004;7:127–133. Available at: https://www.tandfonline.com/doi/abs/10.1080/14647270410001699081 [Last accessed: December 2023].
- National Health Service. What happens: IVF. Available at: https://www.nhs.uk/conditions/ivf/what-happens/ [Last accessed: December 2023].
- van der Linden M, Buckingham K, Farquhar C, Kremer JAM, Metwally M. Luteal phase support for assisted reproduction cycles. Cochrane Database of Systematic Reviews 2015. Available at: https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD009154.pub3/full [Last accessed: December 2023].
- National Health Service. Availability: IVF. Available at: https://www.nhs.uk/conditions/ivf/availability/ [Last accessed: December 2023].
- Human Fertilisation and Embryology Authority. Intrauterine insemination (IUI). Available at: https://www.hfea.gov.uk/treatments/explore-all-treatments/intrauterine-insemination-iui/ [Last accessed: December 2023].
- Human Fertilisation and Embryology Authority. Intracytoplasmic sperm injection (ICSI). Available at: https://www.hfea.gov.uk/treatments/explore-all-treatments/intracytoplasmic-sperm-injection-icsi/ [Last accessed: December 2023].
- van Loendersloot LL, van Wely M, Limpens J, Bossuyt PMM, Repping S, van der Veen F. Predictive factors in in vitro fertilization (IVF): a systematic review and meta-analysis. Human Reproductive Update 2010;16:577-589. Available at: https://academic.oup.com/humupd/article/16/6/577/740269 [Last accessed: December 2023].
- Bhattacharya S, Maheshwari A, Mollison J. Factors Associated with Failed Treatment: an Analysis of 121,744 Women Embarking on Their First IVF Cycles. Plos One 2013;8: e82249. Available at: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0082249#s4 [Last accessed: December 2023].
- National Institute for Health and Care Excellence. The importance of 3 full cycles of IVF, 2014. Available at: https://www.nice.org.uk/news/blog/the-importance-of-3-full-cycles-of-ivf#:~:text=Most%20women%20typically%20see%20success,pregnancy%20to%2045%2D53%25. [Last accessed: December 2023].
- Copp T, Nickel B, Lensen S, Hammarberg K, Lieberman D, Doust J, Mol BW, McCaffery K. Anti-Mullerian hormone (AMH) test information on Australian and New Zealand fertility clinic websites: a content analysis. BMJ Open 2021;11:e046927. Available at: https://bmjopen.bmj.com/content/11/7/e046927 [Last accessed: December 2023].
- Thomas S, Acharya M, Muthukumar K, Chandy A, Kamath MS, Aleyamma TK. Effectiveness of Anti-Mullerian Hormone-tailored Protocol Compared to Conventional Protocol in Women Undergoing In vitro Fertilization: A Randomized Controlled Trial. Journal of Human Reproductive Sciences 2018;11:24-28. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5892099/ [Last accessed: December 2023].
- National Health Service. Overview: IVF. Available at: https://www.nhs.uk/conditions/ivf/ [Last accessed: December 2023].
- Heffner LJ. Advanced Maternal Age – How Old Is Too Old? New England Journal of Medicine 2004;351:1927-1929. Available at: https://www.nejm.org/doi/10.1056/NEJMp048087 [Last accessed: December ].
- Human Fertilisation and Embryology Authority. Fertility treatment 2019: trends and figures. Available at: https://www.hfea.gov.uk/about-us/publications/research-and-data/fertility-treatment-2019-trends-and-figures/ [Last accessed: December 2023].
- Boedt T, Dancet E, Fong SL, Peeraer K, De Neubourg D, Pelckmans S, van de Vijver A, Seghers J, Van der Gucht K, Van Calster B, Spiessens C, Matthys C. Effectiveness of a mobile preconception lifestyle programme in couples undergoing in vitro fertilisation (IVF): the protocol for the PreLiFe randomised controlled trial (PreLiFe-RCT). BMJ Open 2019;9: e029665. Available at: https://bmjopen.bmj.com/content/9/7/e029665.abstract [Last accessed: December ].
- Van Heertum K, Rossi B. Alcohol and fertility: how much is too much?. Fertility Research and Practice 2017;3. Available at: https://fertilityresearchandpractice.biomedcentral.com/articles/10.1186/s40738-017-0037-x [Last accessed: December 2023].
- Rudick B, Ingles S, Chung K, Stanczyk F, Paulson R, Bendikson K. Characterizing the influence of vitamin D levels on IVF outcomes. Human Reproduction 2012;27:3321–3327. Available at: https://academic.oup.com/humrep/article/27/11/3321/807686 [Last accessed: December 2023].
- Budani MC, Tiboni GM. Effects of Supplementation with Natural Antioxidants on Oocytes and Preimplantation Embryos. Antioxidants 2020;9. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7402117/ [Last accessed: December 2023].
- National Health Service. Risks: IVF. Available at: https://www.nhs.uk/conditions/ivf/risks/ [Last accessed: December 2023].
- Human Fertilisation and Embryology Authority. Risks of fertility treatment. Available at: https://www.hfea.gov.uk/treatments/explore-all-treatments/risks-of-fertility-treatment/ [Last accessed: December 2023].
- How many IVF cycles can I have. Available at: https://www.nhs.uk/conditions/ivf/availability/

